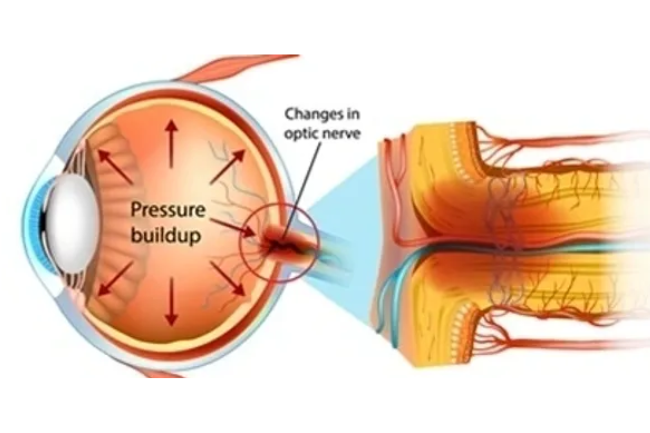
Glaucoma is a chronic eye condition that affects the optic nerve, leading to progressive vision loss if left untreated. It is often associated with increased intraocular pressure (IOP) due to impaired fluid drainage from the eye. Glaucoma typically has no symptoms in its early stages and can go unnoticed until significant vision loss occurs. Risk factors for glaucoma include age, family history, ethnicity, and certain medical conditions. Treatment options may include eye drops, oral medications, laser therapy, or surgery to lower the IOP and preserve vision. Early detection, regular eye exams, and timely intervention are crucial in managing glaucoma and preventing irreversible vision loss.
Glaucoma
What is Glaucoma?
Risk Factors for Glaucoma
- Age: The risk of developing glaucoma increases with age, especially after the age of 40. The risk becomes significantly higher after the age of 60.
- Family History: Having a first-degree relative (such as a parent or sibling) with glaucoma increases the risk of developing the condition.
- Ethnicity: People of African, Hispanic, and Asian descent are at higher risk of developing certain types of glaucoma compared to individuals of other ethnicities.
- Medical Conditions: Certain medical conditions, such as diabetes, high blood pressure, and cardiovascular diseases, can increase the risk of glaucoma. Individuals with a history of eye injuries or surgeries, and those with thin corneas, are also at higher risk.
It’s important to note that having one or more risk factors does not necessarily mean that an individual will develop glaucoma, but regular eye exams and early detection are essential in identifying the condition and managing it effectively.


Common symptoms of Glaucoma
- Gradual loss of peripheral vision: Glaucoma often leads to a gradual reduction in the ability to see objects on the sides or in the periphery of the visual field.
- Blurred or hazy vision: Glaucoma may cause blurred or hazy vision, especially in the later stages of the disease.
- Increased sensitivity to light: Some people with glaucoma may experience increased sensitivity to light or glare.
- Eye pain or discomfort: In some cases, glaucoma may cause eye pain, redness, or discomfort, particularly during episodes of increased intraocular pressure.
It’s important to note that these symptoms can vary depending on the type and stage of glaucoma, and some people may not experience any symptoms at all. Regular eye exams and early detection are crucial in identifying and managing glaucoma effectively.
Routine investigations for Glaucoma
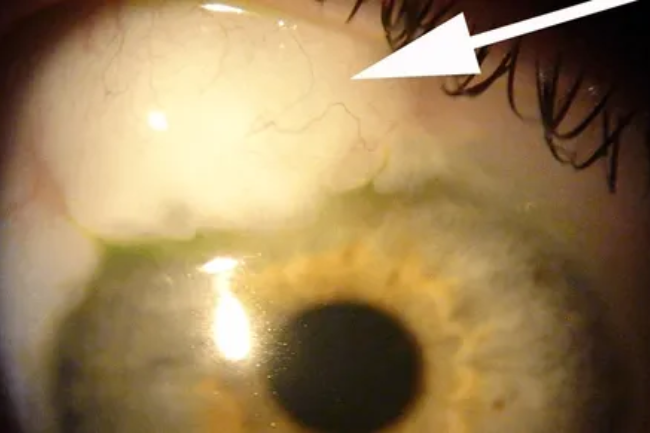
- Tonometry: This is a test to measure intraocular pressure (IOP), which is a key risk factor for glaucoma. It involves using a device to measure the pressure inside the eye.
- Visual field testing: Also known as perimetry, this test assesses the patient’s field of vision to detect any peripheral vision loss, which is a common sign of glaucoma.
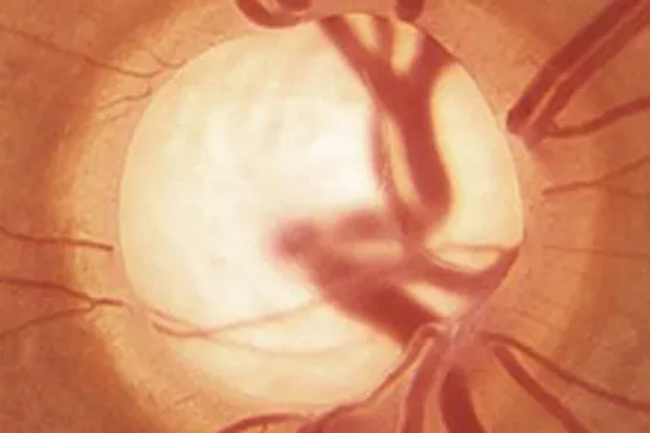
- Optic nerve head evaluation: An ophthalmologist may use a special instrument called an ophthalmoscope to examine the optic nerve head at the back of the eye. Changes in the appearance of the optic nerve head can indicate glaucoma.
- Gonioscopy: This test is done to assess the drainage angle of the eye, which is important in determining the type of glaucoma. It involves using a special lens to view the drainage angle and assess its structure and function.
These routine investigations are commonly performed during a comprehensive eye examination to evaluate the presence and progression of glaucoma, and to guide the management and treatment plan.

Special investigations
- Optical Coherence Tomography (OCT): This imaging technique uses light waves to create detailed cross-sectional images of the retina and optic nerve, allowing for early detection and monitoring of glaucoma-related changes.
- Visual field testing: Advanced visual field tests, such as Frequency Doubling Technology (FDT) and Humphrey Visual Field (HVF) tests, can provide more detailed and sensitive assessments of the patient’s visual field, helping to detect and monitor glaucoma-related visual field loss.
- Imaging of the optic nerve head: Scans such as Heidelberg Retina Tomography (HRT) and Confocal Scanning Laser Ophthalmoscopy (CSLO) can provide detailed images of the optic nerve head, helping to assess the structure and changes associated with glaucoma.
- Genetic testing: In some cases, genetic testing may be recommended to identify specific gene mutations associated with glaucoma, particularly in cases of early-onset or familial glaucoma.
These special investigations may be used in addition to routine tests to provide further insights into the diagnosis, management, and monitoring of glaucoma, depending on the individual patient’s condition and needs.
Medical and Surgical treatment
- Medications: Eye drops or oral medications may be prescribed to lower intraocular pressure, the primary modifiable risk factor for glaucoma. These may include prostaglandin analogs, beta-blockers, alpha agonists, and carbonic anhydrase inhibitors, among others.
- Laser therapy: Laser trabeculoplasty and laser peripheral iridotomy are common laser procedures used to help reduce intraocular pressure in glaucoma patients. These procedures are typically performed in an outpatient setting and can be effective in some cases.
- Surgical interventions: When medication and laser therapy are not effective in controlling intraocular pressure, various surgical procedures may be considered, such as trabeculectomy, glaucoma drainage implants, and minimally invasive glaucoma surgeries (MIGS) like trabecular meshwork bypass stents.
- Combination therapies: In some cases, a combination of medications, laser therapy, and surgical interventions may be used to effectively manage glaucoma and lower intraocular pressure to prevent further optic nerve damage.
The choice of treatment approach will depend on the severity of the glaucoma, the patient’s overall health, and the preferences of the treating ophthalmologist, tailored to the individual needs of the patient.